by Jane Baker Segelken, MA, MSW, part of the Social Work team at Hospicare & Palliative Care Services
Many of us are familiar with the statement “hospice isn’t about dying, hospice is about living.” But what does that really mean? When I first became involved with hospice, I quickly realized it’s about quality of life, now and in the future. Hospice is about living the time at the end of our lives with the least amount of pain and discomfort.
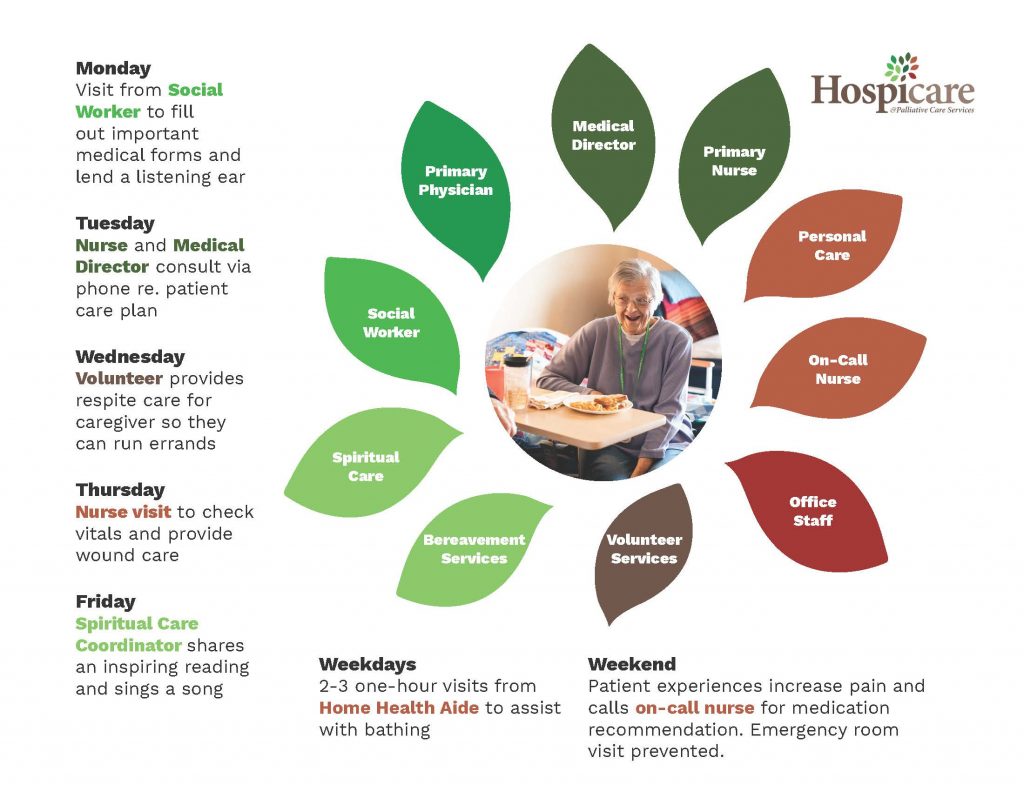
For individuals with a terminal illness, hospice — specifically our local Hospicare serving Cortland and Tompkins counties — shifts the emphasis from allowing our medical conditions to dictate how we live to making those decisions on our own and with a team of support. Utilizing a holistic approach that includes the medical director, nurses, aides, social workers, chaplains, and volunteers, Hospicare works to meet the needs of patients and their family and friends.
Correcting Misconceptions
People often may not get the care they need at the end of life because they have a wrong idea about what hospice means. Many of those I knew who became part of the hospice program were slow to get there, in part because they had an impression that didn’t match reality and saw receiving hospice care as giving up. Hospice care is quite the opposite of giving up; it’s all about offering the highest quality of life-giving care as one faces death. Here are some of the facts about hospice care:
- Your primary care physician and others that offer you care can stay as involved as you want throughout your journey. The staff at Hospicare can serve as principal caregivers or they can support the services you’re receiving elsewhere.
- Hospice isn’t as expensive as many believe. Rather, many of the costs are covered under Medicare, Medicaid, and most private insurance plans and managed care organizations. No one is ever turned away for inability to pay.
- You’ll receive hospice services in the setting that is best for you: a private home, hospital, nursing home, or the Hospicare residence on South Hill in the town of Ithaca.
- There is no limit to how long someone can continue to stay enrolled, although a life expectancy of six months or less is generally required to start hospice services. Although not the norm, there have been cases where someone received hospice services for a year or longer.
- Family, friends, and caregivers can take advantage of many of the opportunities the Hospicare team provide — hospice services aren’t just for the patient. Friendly volunteers can offer respite to the primary caregivers, and aides can help with errands, cooking, and light housekeeping. Hospicare also provides counseling services, educational programs, and support groups to those who are grieving regardless of whether the deceased received hospice services or not.
When Hospice Might Be The Right Choice
An early referral to hospice — before the situation becomes critical — has so many advantages. The patient and loved ones can take advantage of the many services available including the company of trained volunteers who will do friendly visiting, play music, share hobbies, and offer respite to the caregivers. Signing on early also means that the patient can receive specialized nursing care and medications, medical equipment, and supplies sooner than they might have otherwise. Individuals can self-refer to Hospicare when they’re ready. Anyone can contact Hospicare to begin the referral process; it does not have to begin with a physician.
It’s also important to know that if you change your mind and decide that hospice isn’t the right approach for you at the moment or that you’d like to pursue treatment aimed at curing your disease, you can sign off hospice services. If at a later date you change your mind again, a simple phone call can restart the referral process.
Hospice is About Living
Choosing hospice is a shift from disease maintenance and fighting a health condition to focusing on quality of life. It’s not allowing a medical condition to dictate life choices, but instead putting those choices in your hands. Most of all, choosing hospice means that individuals can live their full rich life until the end — and that they don’t have to die alone, afraid, or in pain.
Choosing hospice is not a death sentence. It is life affirming.
To learn more, call the Hospicare admissions staff at 607-272-0212.